Fractures and the importance of bone health
Posted on 6th December 2022 at 09:41
By Carl Green
This post will provide key information on the structure and function of our skeleton, the importance of bone health, types of fractures, and general fracture prevention advice. If you are interested in learning more about other types of musculoskeletal conditions, please take a look at my other posts in this series, of which this is the sixth.
What are bones made of, and why do we have a skeleton?
Bones are made of minerals and collagen (a protein based connective tissue), and have a rich supply of blood vessels and nerves. The outer part of our bones is largely made of densely structured compact or “cortical” bone, and the centre contains a matrix of “trabecular” or “cancellus” bone.
Our bones and skeleton provide bodily structure and stability (with each bone held together by ligaments, protection to vital organs (e.g. rib cage, pelvis, and skull), production of blood cells in the bone marrow of long bones, and anchor points for our soft tissues to facilitate movements (i.e. our muscles pull on our bones via their tendon attachments).
Bone growth and health
Our bones grow in size/length via “growth plates” at the ends of the bones until skeletal maturity (approximately mid 20’s), but then continue to adapt throughout our lifetime. Therefore, our bones should not be seen as dry, brittle and unchanging tissue, but as living parts of our bodies that can fine tune themselves in response to our behaviour.
Within our bones, there are special cells called osteoclasts and osteoblasts, which remove, replace, and reinforce parts of our bone structure in response to the stresses placed on it. This process is called bone remodelling and relies on nourishment (food/drink intake and bodily reserves), various hormones, as well as physical forces being placed on the bone. These physical stresses give our bodies the information they need to understand how to strengthen to better resist similar forces in the future.
So, if a person was inactive with minimal stresses going through their bone structure, their body would adapt to this in a negative way making the bone less capable of dealing with physical forces and more prone to problems. Whereas if that same person were to gradually increase the stresses placed on the bone over time, the body would adapt and create stronger connective skeletal structures to withstand similar forces in the future making that person less at risk of bone problems.
Common types of fractures
Firstly, the words fracture, break, or crack in regard to bones, all essentially mean the same thing, i.e. damage to bone tissue causing it to separate.
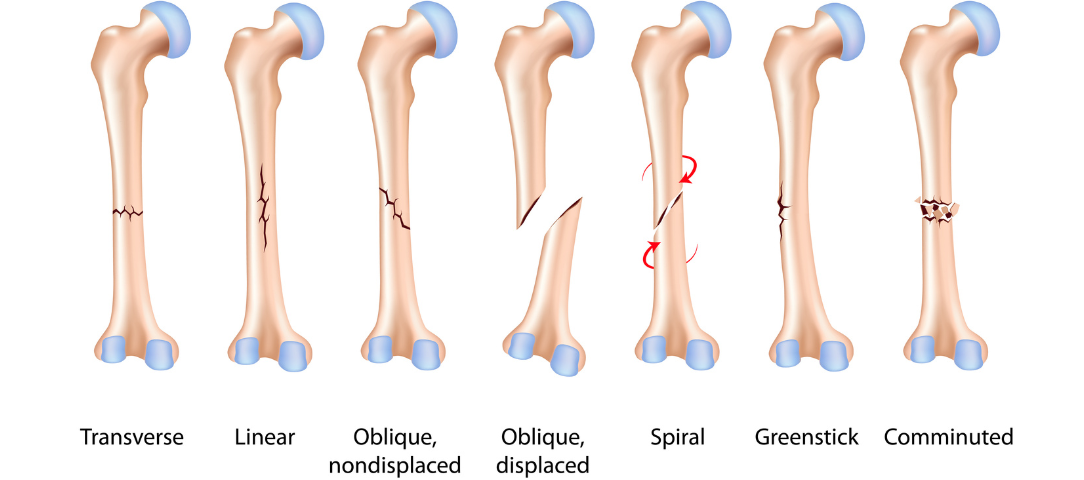
There are many terms to help categorise different types of fractures, however terminology can be confusing or misleading if used or interpreted by those unfamiliar with the terms. So, here are 12 of the most common examples that came to mind (also see the image on this page) with my brief explanation of each, to help you make sense of the common types of fracture terms you may come across…
1. Non-displaced fracture – bone has broken but stayed in correct alignment (more likely to heal)
2. Displaced fracture – bone has broken and rotated, tilted or shifted out of alignment (unlikely to heal, also known as a malunion, unless the fractured bone surfaces are held together)
3. Closed fracture – bone has broken but not pierced the skin, and is therefore not visible
4. Open fracture – bone has broken and torn through the skin and underlying tissue, so is visible. Sometimes this is also called a compound fracture.
5. Osteoporotic fracture – bone that has broken due to weakened bone density which can be caused my poor nutrition, hormone changes (e.g. post menopausal) and insufficient weight bearing exercise, usually triggered by a compressive or impact stress (but not necessarily a big injury).
6. Pathological fracture – bone has been broken/damaged by another health conditioning such as a tumour or tuberculosis
7. Avulsion fracture – bone has been broken by a pulling force from a connecting ligament or tendon. Can happen during a sprain or strain injury in someone who has stronger soft tissue than bone
8. Stress fracture – bone weakened through overloading with inadequate recovery, and possibly nutrition or metabolic and hormonal issues, leading to separation/fracture
9. Green-stick fracture – incomplete traumatic fracture in childhood (when bones are more flexible so don’t separate fully)
10. Transverse or oblique fractures – bone breaks all the way through in a straight horizontal (transverse) or diagonal (oblique) line due to traumatic injury
11. Spiral fracture – bone breaks all the way through in a spiral/corkscrew shape, usually due to a twisting injury either in weight bearing or with the bone fixed/trapped in position.
12. Comminuted fracture – where the bone breaks in multiple places creating bony fragments rather than a single break/fracture line, usually caused by a crush injury
How to realistically reduce your risk of fracture
Through considering all the information we have covered so far, we can logically plan ways to improve our bone health and reduce risk of injury (fracture). Here is a brief list of behaviours that could be beneficial…
· Ensure your day includes at least a few hours of weight-bearing activity (e.g. any combination of standing, walking or exercise)
· Complete gradually progressive strength training exercises (within your capabilities) at least twice a week covering all major muscle groups (e.g. push, pull, lift and carry) or more specific programmes for those with higher level demands (such as manual work or sport)
· Consume enough energy/calories, protein, calcium, magnesium, phosphorus, potassium, vitamin D, and vitamin C for your situation (be aware that your health, activity levels, skin tone, and daylight exposure can influence what you need)
· Ensure you build up all physical activities gradually and monitor for any warning signs of overloading and over training such as fatigue, pain/aching, and swelling
· Postmenopausal women experiencing problems may want to consider speaking to their GP about supplements and possible hormone replacement therapy
· Being mindful of potential causes for injury during day-to-day life and sporting activities to reduce the risk of putting ourselves in harmful situations (although not all traumatic injuries are avoidable, and unfortunately can be just part of life)
What’s next?
If you have any questions or are interested in our support, please get in touch with us at Colchester Physiotherapy and Sports Injuries Clinic, and myself (Carl Green) or my physiotherapist colleagues Craig Fowlie or Jane Marr will do all we can to help you.
The topics I’ll be writing about next in my “musculoskeletal conditions” series instalment will be tendinopathies and bursitis, so check back in for that or follow us on social media to see when it is published.
Treatment and Rehabilitation at Colchester Physiotherapy & Sports Injury Clinic
If you are having issues with any of the different types of musculoskeletal conditions we would advise you to speak to a professional. Our team are experts in treatment and rehabilitation of musculoskeletal injuries or problems, and can offer you practical and effective advice on how to avoid or deal with a wide range of musculoskeletal conditions. If you require any more information about our services, reach out today or give us a call on 01206 579631.
Get in touch with the team here at Colchester Physiotherapy and Sports Injury Clinic for honest advice and recommendations!
Other Articles in our Musculoskeletal Condition Series
Author
Carl Green

Carl is a Specialist Musculoskeletal Physiotherapist, Sports Science and Human Biology graduate, former Lecturer in Sport and Exercise, Personal Trainer, and Sports Massage Therapist.
He has worked as a Physio within the NHS at a senior level, sports injury clinics, his own practice, stroke rehabilitation, occupational health and chronic pain. Carl also has first hand experience of acute and chronic injuries, pain, surgery, and disability, giving him a deeper understanding how these can affect us both physically and psychologically.
He started his career in health and fitness in 2002. Empowering people to achieve their goals, overcome challenges, and reduce future problems through lifestyle/behaviour change and exercise has continued to be a big part of his approach as a Physio.
Carl has tried many sports, but mainly focused on rugby, gym training, running (5k to half marathon), and Muay Thai Boxing. He also enjoys snowboarding, home gym training, teaching his dog tricks and playing fetch, covering songs on his guitar, and has recently taken up archery.
Tagged as: Musculoskeletal Condition Series
Share this post: